Hiv And Periodontal Disease
Hiv and periodontal disease. It can take two forms. HIVAIDS is a serious medical condition that can have certain dental symptoms. Chronic dry mouth gingivitis bone loss around the teeth periodontitis canker sores oral warts fever blisters oral candidiasis thrush hairy leukoplakia which causes a rough white patch on the tongue and dental caries.
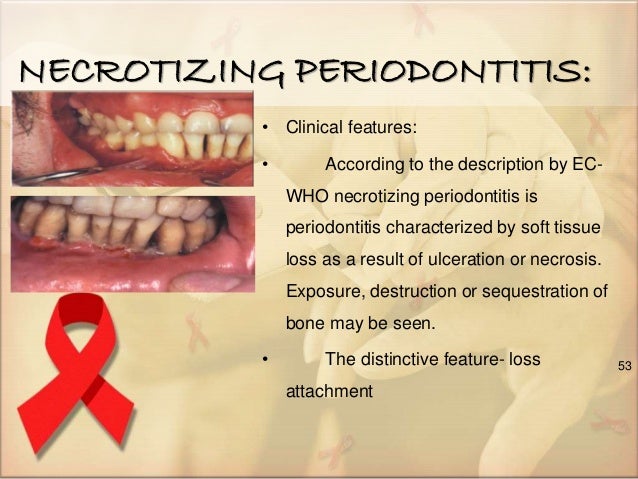
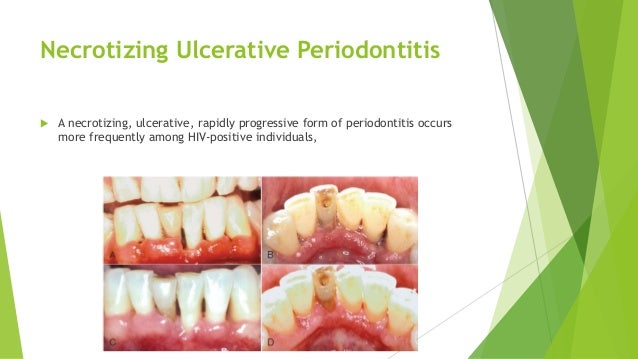
The immunosuppression resulted by the HIV infection can justify the high frequency and the difficult in controlling the CP in this group of patients raising the possibility of additional factors associated to the development of CP in HIV patients. The rapid and severe condition called necrotizing ulcerative periodontitis NUP and its associated and possibly precursor condition called linear gingival erythema LGE. Clearly immunosuppression can potentiate PD as evidenced by reports of florid examples of HIV-associated gingivalperiodontal disease during the early days of HIV outbreak in the United States 34.
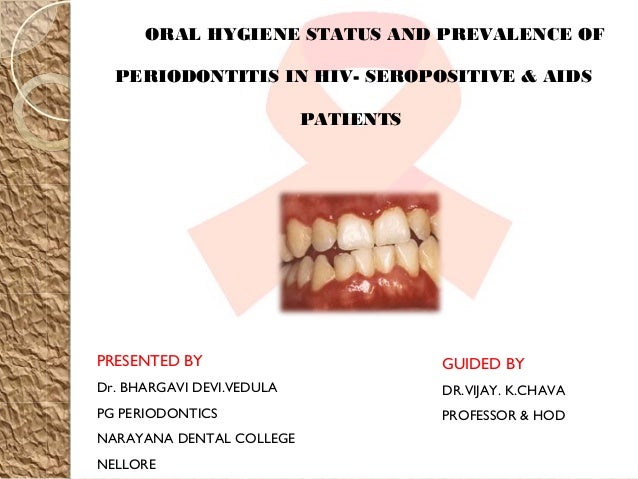
Periodontal diseases such as chronic periodontitis CP frequently occur in immunosuppressed patients including HIV-infected patients. Between CD4 count and gingivalperiodontal status or attachment loss with HIV staging. Most common are Kaposis sarcoma and non-Hodgkins lymphoma.
While HIV-positive adults appear to be at increased risk for more severe periodontal disease there are no studies address-ing this relationship in children. Dental caries tooth decay periodontal diseases oral cancers oral manifestations of HIV oro-dental trauma cleft lip and palate and noma severe gangrenous disease starting in the mouth mostly affecting children. Periodontal disease associated with HIV infection.
Some of the most common oral problems for people with HIVAIDS are. Concomitant dental diseases especially caries and periodontal disease has been reported in HIV-positive children. Department of Health and Human Services HHS as part of an award totaling 1000000 with 0 financed with non-governmental sources.
Periodontal disease is a fairly common problem in both asymptomatic and symptomatic HIV-infected patients. Oral hygiene using mechanical therapy improves the gingival condition suggesting that it is an important step in the maintenance of. Chronic gingivitis was the most frequent disease in HIV infected and AIDS patients.
It is possible that certain factors may increase a persons chances of getting HIV or other STDs during oral sex if exposed to an infected partner such as. Having poor oral health which can include tooth decay gum disease or bleeding gums and.
Concomitant dental diseases especially caries and periodontal disease has been reported in HIV-positive children.
The majority of oral health conditions are. Chronic dry mouth gingivitis bone loss around the teeth periodontitis canker sores oral warts fever blisters oral candidiasis thrush hairy leukoplakia which causes a rough white patch on the tongue and dental caries. Effect of highly-active antiretroviral therapy. There is a need to update and revise the classification criteria for diag-nosis of oral manifestations in children with HIV infection to include data from Africa Asia and India. Periodontal disease associated with HIV infection. The immunosuppression resulted by the HIV infection can justify the high frequency and the difficult in controlling the CP in this group of patients raising the possibility of additional factors associated to the development of CP in HIV patients. Periodontal disease is a fairly common problem in both asymptomatic and symptomatic HIV-infected patients. The majority of oral health conditions are. It can take two forms.
It can take two forms. Concomitant dental diseases especially caries and periodontal disease has been reported in HIV-positive children. Patients with severe immunosuppression as a consequence of infection by human immunodeficiency virus HIV are at risk for a number of severe periodontal diseases. Neoplasias may also involve the periodontium. While periodontal disease can occur in anyone regardless of HIV status one particularly severe form necrotizing ulcerative periodontitis and a. Clearly immunosuppression can potentiate PD as evidenced by reports of florid examples of HIV-associated gingivalperiodontal disease during the early days of HIV outbreak in the United States 34. The rapid and severe condition called necrotizing ulcerative periodontitis NUP and its associated and possibly precursor condition called linear gingival erythema LGE.



































Post a Comment for "Hiv And Periodontal Disease"